Do you see floating objects in your vision?
Learn more about floaters
What Are Floaters?

Vision with floaters

Normal vision
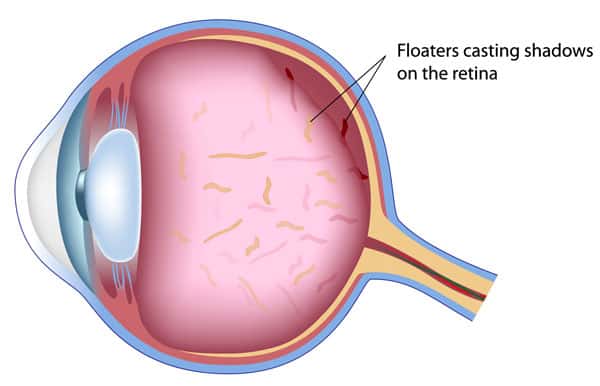
Eye vitreous floaters occur when the collagen in the vitreous gel starts to break down as we age, this usually begins around the ages of 50 to 60 years. Overtime, the collagen thickens and forms clumps. The movement of these clumps cast little shadows on the retina, giving rise to what we perceive as “floaters”.
- Floaters come in various forms, shapes and sizes
E.g. little black dots, hair-like forms, worms, strings or ropes, or even small fly-like insects - Floaters may appear in and disappear out of your vision
- Floaters are usually more noticeable when viewed against a light or uniform background
Are Floaters Harmful? Should You Be Concerned?

Floaters are part of the eye’s normal ageing process and are generally not harmful. However in certain cases, floaters can co-exist with retinal tears and retinal holes. There is a rapid increase in floaters when this happens. The extent of floaters can be so significant that it appears as a dense fog.
Floaters, whilst a common symptom, require a thorough eye examination by an ophthalmologist to ensure that you do not have retinal tears or other more sinister eye conditions, as some of these can be treated.
Are You Experiencing an Increase in Eye Floaters?
Prevent, detect and treat early for a better everyday life.
During your consultation with an ophthalmologist, one or more of the following clinical assessments will be done:
| 1. Visual acuity test This involves getting you to read letters on a testing chart. |
|
| 2. Measurement of pressure within your eye This may be tested either by an air puff, involving a small gust of air directed transiently on the eyeball for a fraction of a second, or a contact measurement technique using a device placed on the eye for 1 or 2 seconds. |
|
| 3. Measurement of the refractive status of your eye It allows us to determine if your vision would be further improved with a spectacle prescription. |
|
| 4. Slit-lamp examination Your eye doctor will examine your eye for retinal holes and tears. |
|
| 5. Dilated examination of the back section of your eye After dilating eye drops are instilled into your eye, the ophthalmologist will examine your eye for retinal holes and tears, and to ensure the retina is in a good position. |
Further tests may be performed depending on your other symptoms and the initial assessments conducted by our eye specialist.
Your eye specialist will then discuss with you whether any immediate treatment is required.
Why LSC Eye Clinic?
| Appointment making is easy and fast | Retina specialist with international experience | Conveniently located right at the heart of Orchard | 15 years of helping patients care for their eyes |

Frequently Asked Questions
- Please avoid wearing contact lenses on the day of your eye check. We recommend that you wear your glasses.
- It is recommended that you set aside 2 to 3 hours for your appointment.
- You will also be advised not to drive after your eye screening as eye drops will be instilled to dilate the pupils of your eyes and that may blur your vision for 4 to 5 hours. Clarity of distance vision is largely unaffected but you will experience more glare. You will most likely resume normal vision within the next 12 to 24 hours.
There are numerous suggestions on getting rid of vitreous floaters, including relaxation techniques such as yoga and meditation. Whilst these may help with managing the psychological impact of floaters, physical reduction or removal of floaters is only possible with medical treatment.
The medical treatment options are:
- YAG Laser Vitreolysis
The YAG laser vitreolysis procedure involves a disruptive laser which is directed at a large floater particle, delivering enough energy to fragment the floater into little bits. Very often, the little bits become dispersed, and patients can still be symptomatic from the procedure. So while some patients may indeed have improved symptoms, on average, the outcomes with this procedure can be somewhat unpredictable, and more than 1 treatment session may be needed. Also, the large amount of energy introduced into the eye in a fairly unregulated manner can potentially cause retinal damage.
- Vitrectomy Surgery
The surgical treatment of floaters is known as vitrectomy (sometimes nicknamed “floaterectomy”). Vitrectomy is a commonly-performed surgical procedure, but usually for other reasons, i.e. to reattach a detached retina, or remove membranes on the retina, rather than to remove floaters per se. It is essentially a micro-incision surgical procedure performed under local anesthesia. It is an outpatient procedure that usually takes less than 1 hour. The retinal surgeon will remove the vitreous gel completely, and along with it all the floater debris. The efficacy of this procedure to remove floaters is undoubted, and patients will have complete eradication of floaters after the procedure. The main consideration in deciding whether a patient should undergo this procedure, is that there lies a 3-5%, i.e. small but not negligible risk of causing visual complications, which cannot be eventually corrected with glasses. Most important amongst these complications are retinal detachments arising from retinal tears caused by the vitrectomy procedure. Retinal detachments are sight-threatening and will require surgery to reattach the retina. In patients who have not yet had cataract surgery, a vitrectomy will also accelerate cataract development, and so patients would need to accept that cataract surgery might be needed at some point in the near future.
Request for an Appointment
Tel: +65 6836 1000
Whatsapp: +65 9843 1000
For general enquiries and appointment only
Email: [email protected]
Monday to Friday: 9am to 6pm
Saturday: 9am to 4pm
*Last Registration Time 2pm
Sunday & PH: Closed

 +65 6836 1000
+65 6836 1000