What is a macular hole?
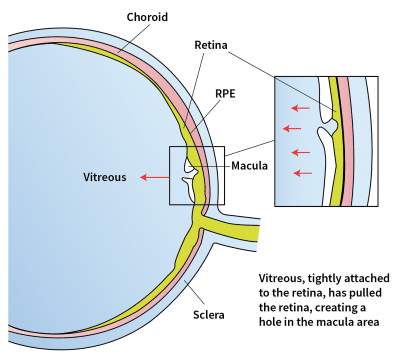
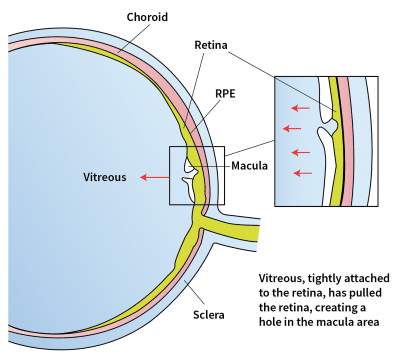
A macular hole is a small break occurring in the centre of the retina. The centre of the retinaThe retina is the thin layer of nerve tissue lining the back of the eye that detects light and sends information to the brain to allow us to see. is the macula, and this area is responsible for precise vision, allowing us to appreciate fine detail, contrast, and colour.
What causes a macular hole?
As part of the natural ageing process in the eye, the vitreous gel gradually shrinks and pulls away from the retina. This process creates abnormally high forces on the macula. If these forces are strong enough, they create a macular hole.
Other factors also increase the chances of developing a macular hole:
- High degrees of short-sightedness
- Retinal detachment
- Prior eye trauma
- Macular swelling from diabetes or macular degeneration
What are the visual symptoms of a macular hole?

Normal vision

Vision with macular hole
A macular hole causes blurry vision or a distinct darkish spot in central vision. This affects reading, driving and performing tasks that require seeing fine details. A macular hole does not lead to a complete wipe-out of vision as it only affects central vision. The peripheral (i.e. side) vision will remain intact and unaffected.
It is possible that both eyes are affected by macular holes.
Can a macular hole heal on its own?
Early macular holes may resolve on their own, over a course of a few months. However, for the majority of macular holes, surgical treatment to close the macular hole is required in order to improve vision.
Every patient with a macular hole requires assessment by an eye specialist to understand the natural course of the disease and potential treatment options.
Speak to an eye specialist in Singapore today.
How do retinal surgeons treat macular holes?
Macular holes are treated with a micro-incision surgical procedure called vitrectomy that usually takes 1 hour. This procedure can be performed under local or general anaesthesia.
During vitrectomy surgery, the vitreous gel is removed, which relieves the tension caused by the gel tugging on the macular hole. Tension around the macular hole is also relieved. For larger or longer-standing macular holes which are more difficult to close with these strategies alone, your retinal surgeon may additionally use membrane or lens capsule grafts to plug the hole. A gas bubble is placed in the vitreous cavity. After the surgery, the bubble remains in contact with the macula to facilitate closure of the macular hole.
A few days of face-down head positioning is usually required after macular hole surgery, which will allow the bubble to support the macula and assist in hole closure. This is usually the hardest part of the post-operative recovery!
If a gas bubble is placed in your eye, you must not travel by air or travel to high altitude locations until the gas bubble is completely gone. This is because the gas bubble will expand in size and can lead to increased pressure inside the eye and cause visual loss.
Silicone oil may also be used in lieu of gas, if there are specific reasons to, i.e. if you need to travel by air very soon after surgery, or difficulty with maintaining a face down position.
Request an Appointment with a Retina Specialist
Consultant
MBBS, MMed(Ophth), MRCSEd,
FRCSEd, FRCOphth, FRCS(Glasg), FAMS, FRCS(Canada)
Subspecialty: Cataract surgery, general ophthalmology, macular degeneration, diabetic eye disease, vitreoretinal surgery, uveitis
Senior Consultant
MBBS (Singapore), M.Med (OPHTH),
FAMS (Ophth), MCI (SINGAPORE),
PHD (UTRECHT)
Subspecialty: Retinal conditions, floaters & flashes in vision, age-related macular degeneration, myopia in children & adults, cataracts
Frequently Asked Questions
The success rate for hole closure, and visual recovery after vitrectomy depends on many factors and may vary with each individual. You should discuss these with your eye doctor.
Overall, there is a greater than 95% chance of closing the macular hole with vitrectomy surgery.
Regarding vision: the vast majority of patients who have had closed holes following surgery have an improvement in their vision. However, as the recovery of vision depends on how the nerve fibers heal, and can be suboptimal in a small percentage of patients, there is a small chance that vision may not improve after surgery, even if the hole is closed. Usually, these patients would have had a long- standing macular hole, or underlying conditions in the macula, such as macular edema.
Just like every other surgical procedure, there are several important risks and potential adverse events that are associated with vitrectomy. The more common risks include:
Cataract formation and progression:
If you have not had cataract surgery, a macular hole vitrectomy operation will accelerate the development of a cataract. This occurs in every patient who has had vitrectomy surgery. Cataracts can progress and if they impact your vision significantly, then you may require cataract surgery.
Raised eye pressures:
In the first few days after surgery, the pressure within your eyeball may be high, most commonly because of gas injected into the eye. This would usually settle with the use of intraocular pressure drops. These eye drops can be used for short-term, until the pressure is stabilised. Later increases in intraocular pressure can occur as a result of the use of steroid eye drops, which are prescribed routinely after surgery, and would usually settle once the steroid drops are stopped.
Rarely after vitrectomy the eye pressure can remain elevated and you may require eye drops on a longer- term basis, or even surgery, to control the eye pressures.
Retinal detachment:
There is a 2-3% risk of a retinal detachment occurring after macular hole surgery. If this occurs, then in order to preserve vision and limit the extent of loss of vision, you would require retinal reattachment surgery, usually a vitrectomy.
Infection:
As with all surgeries involving the eye, there is an inherent risk of an infection (i.e endophthalmitis). The risk of endophthalmitis after vitrectomy surgery is lower than that after cataract surgery.
In the first 2 weeks after surgery, eye pain, discomfort, floaters, and eye redness, especially if not settling and increasing, should prompt an immediate visit for your eye doctor to check on your eye, so that early injection of antibiotic treatment into the eye can be administered. If the infection is severe, then vitrectomy surgery to remove infective material from the eye may be required to treat the infection.
There are other intraoperative risks and post-operative risks aside from the above mentioned. Your retinal surgeon will discuss with you regarding the potential benefits of vitrectomy surgery with regards to hole closure success rates and likelihood of visual improvement, and weigh these in relation to the surgical risks.
It is important to recognize that the full extent of visual recovery after vitrectomy for macular hole surgery can take up to 6 to 12 months. Most of the improvement in vision occurs in the first 3 months after surgery.
Initially, your vision will be very poor with the gas in your eye, to the extent that you will only be able to count fingers. As the gas disperses and is replaced by your eye’s natural fluid, you will begin to see a line, which wobbles in your vision. This line indicates the meniscus of the gas bubble.
You will be able to see above the line, but the vision will be fuzzy below this line. Once the meniscus of the gas bubble descends to below the horizontal midline, you will be able to appreciate your true post-operative vision. This will be significantly better than before surgery.
Slight distortion of vision, blurriness in the middle, or reduced contrast ability, may still be present at this point, and will likely improve over the next 4-5 months. You will increasingly feel that your vision with both eyes is more comfortable over time.
With time, the bubble shrinks to leaving only a tiny bubble of gas at the bottom which will eventually disappear.
Cataracts: It may happen during the post-operative recovery period, you will notice that your vision is still fairly blurry. This is most likely due to a cataract, and your surgeon will be able to discuss with you the option of having cataract surgery.



