The Warning Signs of
A Retinal Detachment & What You Should Do
What is a Retinal Detachment?
The retina is the all-important light-sensing structure that lines the back of the eye. It is like the film in a camera, receiving and transmitting light impulses to the brain, allowing us to see.
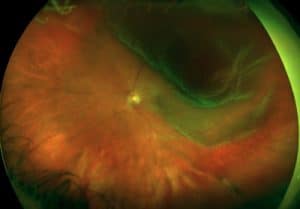
A retinal detachment occurs when the retina separates from the wall of the eye, much like how wallpaper peels off the wall.
Experiencing a retinal detachment can be extremely frightening, with sudden hazy vision littered with hundreds of floaters, persisting flashing lights, and emergence of a dark shadow encroaching onto side vision.
Retinal detachments can potentially cause permanent vision loss if left untreated.
However, with early detection and treatment, it may be possible to restore the same level of vision prior to the retinal detachment treatment or reduce the extent of visual loss.
What Causes It?
The most common form of retinal detachments are rhegmatogenous, i.e. caused by a retinal tear. As we get older, the vitreous gel in our eyes progressively softens and becomes more liquefied. The end point of this process is an acute posterior vitreous detachment, when the vitreous gel suddenly and rapidly peels away from the retina with enough force to cause a retinal tear.
If a retinal tear is left untreated, vitreous fluid passes through it and separates the retina from the wall of the eye, leading to a retinal detachment. Emergency medical care is absolutely required to treat a retinal detachment.
What are the
Warning Signs of a Retinal Detachment?
- Floaters (i.e. hair-like wriggly lines, specks, flecks, fly-like structures)
- Flashing lights
- A shadow starting in your side vision and progressing towards the center
If you have the above symptoms, seek medical attention immediately.
In some individuals with fairly slowly progressing retinal detachments, there may not be any symptoms until the detachment worsens. Hence a comprehensive eye examination by an ophthalmologist is critical, as early retinal detachment treatment would then be possible.



Are You At Risk?
Your risk for a retinal detachment is increased if you:
- Are older
- Are highly short-sighted
- Have degenerative changes in your retina, e.g. lattice degeneration
- Have had prior eye surgery such as cataract surgery
- Have had previous trauma to the eye
- Have a family history of retinal tears or detachment
Retinal Detachment Treatment and Surgery in 4 Main Ways:
The goal of treatment is to reattach the retina and preserve vision. The majority of detachments require retinal detachment surgery, of which there are 4 main types of retinal procedures.
1. Vitrectomy
This is a keyhole procedure where the vitreous gel is removed and retinal tears are treated. It is typically performed under local anesthesia and can take between 45 minutes to 2 hours or more, depending on the complexity of the retinal detachment. A vitrectomy allows the surgeon to repair the detached retina from within the eye.
Three tiny keyholes are made in the white of the eye (i.e., the sclera) to access the vitreous gel. The vitreous gel, which is tugging on the retina, is completely removed, and fluid under the retina is drained. Once the retina is placed back into position, the tear is sealed with either laser or cryotherapy freezing treatment. A gas or oil bubble is placed in the eye to fill the space previously occupied by the vitreous gel, to keep the retina in position in the few weeks to months following the surgery.
Gas, unlike oil, gradually disappears from the eye as it is absorbed into the blood stream. Depending on the type of gas used, this interval may vary from between 2 weeks to slightly more than 3 months. If oil is used, an oil removal procedure will need to be scheduled once the retina is stable and in a good position.
2. Scleral Buckle
The retinal detachment is repaired from exclusively outside the eyeball. A silicone buckle implant is secured to a section of the external eye surface, allowing approximation of the retina to the retinal tear and enhances its closure. The tear is treated with cryotherapy freezing treatment to seal it. A scleral buckle procedure can be performed under general or local anesthesia.
Access to the external eye surface is gained by fine dissection of the conjunctival coverings around the eyeball. The silicone implant is placed and secured to the external eye surface. The tear is then treated with freezing treatment to seal it, and fluid beneath the retina may be drained externally through the eye wall. With the surgery completed, the implant is not visible to an external observer looking at the eye. External small stitches placed in this procedure will dissolve between 4-6 weeks post-surgery.
3. Pneumatic Retinopexy
Pneumatic retinopexy is an option for specific types of retinal detachments, such as cases where the retinal breaks are in the upper two-thirds of the retina. The procedure is performed under local anesthesia, and involves sealing of the retinal tear with cryotherapy freezing treatment or laser retinopexy, and injection of a gas bubble into the eye. The bubble holds the retinal tear closed, and gradually over time the fluid is reabsorbed.
After the procedure, the patient would need to adopt one or more different head positions to keep the bubble in the most optimal position such that the tear remains closed and until the fluid is completely reabsorbed.
4. Laser Retinopexy
Laser retinopexy may be an option for smaller peripheral retinal detachments which are stable, i.e., limited progression over time. Such detachments occur in patients who may not be experiencing any symptoms due to the detached retina, and are discovered on routine comprehensive eye examinations. A relatively low-risk laser procedure is an effective non-surgical option in creating a barricade around the detachment to secure it, and prevent its progression.
For more complex cases, a combination of techniques may be required, e.g. a vitrectomy and scleral buckle, or a scleral buckle and pneumatic retinopexy. Your retinal surgeon would determine which approach is most suitable, weighing the pros and cons of each option, to offer you the highest chance of surgical success.
Frequently Asked Questions
There is a short window of time to treat and seal the retinal tear, before a tear progresses on to a retinal detachment. Thus detachments can be prevented if the tear is sealed in time. If a retinal detachment develops, then in the vast majority of cases, retinal reattachment surgery is required.
Therefore, if you experience any new or increase in floaters, see your ophthalmologist immediately as this may signal a retinal tear, which should be expediently treated!
In general, the choices for the type of retinal surgery depends on several factors, including:
- The exact configuration of the retinal detachment and the tears that are causing it
- Age of the patient
- Whether there is already a cataract present
- The extent of the posterior vitreous detachment
- Other eye conditions such as glaucoma
- Factors such as the ability of the patient to position well, or the need for air travel in the post-operative period
Your retinal specialist would be best able to advise on the best approach in your eye, to ensure the highest possible chances of success.
In general, the rate of successfully reattaching the retina in one surgical operation is in the range of 85 to 90%. Sometimes, more than one surgery is needed, but by and large, more than 99% of patients will have their retinas reattached.
*It is important to note that these numbers are aggregate figures and are determined from large studies of retinal detachments. Every case of retinal detachment is unique, therefore you should speak to your surgeon about the specific assessment of your risk profile and prognosis for success.
The first priority of retinal reattachment surgery is in fact not vision itself, but to return the retina back into position. Following that, visual recovery occurs by way of a gradual establishment of nerve connections that will determine the final level of vision in your eye. The extent of visual improvement depends on whether you have a macular-on detachment (where the macula is still attached), or a macula-off detachment (where the macula has been detached).
- In a macular-on detachment, surgical treatment would usually be able to restore the same level of vision as before the detachment had occurred. The shadow that was present in your vision as a result of the detachment would gradually fade in the weeks after surgery.
- In a macular-off detachment where the macula has been detached for only a short amount of time, then it is potentially possible that the final vision may only be mildly disturbed in terms of color, size, contrast, and distortion of objects, provided surgery is performed early.
- Eyes with a macular-off detachment where the macula has been detached for a fairly long interval may still demonstrate an improvement in vision, however the prognosis of visual recovery after the surgery is certainly more conservative. Nevertheless, fixing a macular-off detachment is important, as it salvages vision and also because without treatment, it would eventually lead to total loss of vision over the course of time.
Overall, the visual outcomes of retinal surgery are good, especially given that these retinal detachments are sight-threatening to begin with.
Meet Our Doctor

Dr Errol Chan
CONSULTANT
MBBS, MMED (OPHTH), MRCSED,
FRCSED, FRCOPHTH, FRCS (GLASG), FAMS
Our ophthalmologist, Dr Errol Chan, has a special interest in vitreoretinal surgery. Dr Chan was awarded scholarship by the Retina Foundation of Canada to pursue a Vitreoretinal Surgery Fellowship at McGill University in Canada, well-regarded for its high-volume retinal surgery program. He was also accepted in the highly-selective Vitreoretinal Surgery Fellowship at the world-renowned Moorfields Eye Hospital London in the UK.

Dr Wong Chee Wai
SENIOR CONSULTANT
MBBS (Singapore), M.Med (OPHTH), FAMS (Ophth),
MCI (SINGAPORE), PHD (UTRECHT)
Dr Wong obtained his Bachelor and Masters degrees from the National University of Singapore (NUS) and completed both his specialist training in ophthalmology and vitreoretinal subspecialty fellowship training for both medical and surgical retina at SNEC. He also completed his Masters in Clinical Investigation at NUS Medicine and a PhD in Ocular Drug Delivery at Utrecht University in the Netherlands. He is a fellow of the Academy of Medicine, Singapore.
Make an Appointment

Tel: +65 6836 1000
Whatsapp: +65 9843 1000
For general enquiries and appointment only
Email: [email protected]
Monday to Friday: 9am to 6pm
*Last Registration Time 2pm
Saturday: 9am to 1pm
Sunday & PH: Closed