What is an epiretinal membrane?
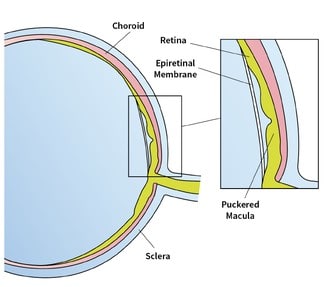
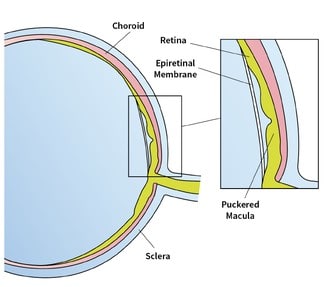
An epiretinal membrane is a retinal condition where a sheet of scar tissue develops across the central part of the retina, an area called the macula.
An epiretinal membrane can affect a person’s central vision. Patients experience distorted and blurred vision, as well as reduction in the level of sight, which can affect reading or recognizing faces.
This condition will not cause total blindness if left untreated. However, if vision is severely affected, it is important to seek medical attention from an eye specialist.
What causes an epiretinal membrane?
An epiretinal membrane is most common in individuals aged 50 years old and above. In most cases, there is no underlying cause for this condition. It is thought that most epiretinal membranes occur because the vitreous gel in the eyeball pulls away from the retina, a common age-related change in the eye.
An epiretinal membrane may be associated with other eye conditions such as:
- Retinal tears or holes
- Retinal vascular diseases e.g. diabetic retinopathy
- Inflammation within the eye
- Prior eye surgeries e.g. laser or cryotherapy treatment and retinal detachment surgery
- Prior eye injuries
Read the Singapore Epidemiology of Eye Disease Study on the prevalence and risk factors for an epiretinal membrane.
Can an epiretinal membrane be treated?
The only treatment method for an epiretinal membrane is its removal by way of a surgical procedure known as a vitrectomy.
Early epiretinal membranes may not necessarily need treatment if the impact on vision and extent of visual distortion is mild. These membranes may progress with time, however, eventually causing a problem with vision. Patients with such membranes may consider treatment.
Should I have surgery for my epiretinal membrane?

Blurry and distorted vision caused by an epiretinal membrane
If your ability to perform daily tasks is affected, the option of surgery should be considered. Such daily tasks include reading and descending stairs, which can be particularly difficult, since these activities require good vision in both eyes.
Your doctor will also be able to discuss the potential benefits of vitrectomy surgery in improving your eye condition, and weigh these in relation to the surgical risks.
An epiretinal membrane can be diagnosed during a routine vision exam. Getting an eye examination at least once in two years is the best way to ensure that your eyes are healthy and that no new eye conditions are developing.
Are you experiencing blurry vision or visual distortion? Get in touch with Dr Errol Chan, our retinal specialist, to have your concerns addressed.
Request an Appointment with a Retina Specialist
Doctor Caring For You
Consultant
MBBS, MMed(Ophth), MRCSEd,
FRCSEd, FRCOphth, FRCS(Glasg), FAMS, FRCS(Canada)
Subspecialty: Cataract surgery, general ophthalmology, macular degeneration, diabetic eye disease, vitreoretinal surgery, uveitis
Senior Consultant
MBBS (Singapore), M.Med (OPHTH),
FAMS (Ophth), MCI (SINGAPORE),
PHD (UTRECHT)
Subspecialty: Retinal conditions, floaters & flashes in vision, age-related macular degeneration, myopia in children & adults, cataracts
Frequently Asked Questions
The epiretinal membrane may not necessarily get worse as it is typically slow in progression. The changes in vision may only be detected over a period of months to years.
There are however some types of epiretinal membranes (i.e. those that develop after retinal detachment surgery) that may progress fairly rapidly. In such cases, your retinal surgeon may recommend surgery in the first instance.
In general, you should only go ahead with surgery if you find the distortion of your vision troublesome, or if there is a rapid deterioration in vision, but not as a preventative measure.
Just like every other surgical procedure, there are several important risks and potential adverse events that are associated with a vitrectomy. The more common risks include:
Cataract formation and progression:
If you have not had cataract surgery, a macular hole vitrectomy operation will accelerate the development of a cataract. This occurs in every patient who has had vitrectomy surgery. Cataracts can progress and if they impact your vision significantly, you may require cataract surgery.
Raised eye pressures:
In the first few days after surgery, the pressure felt within your eyeball may be high due to the gas being injected into the eye. This would usually settle with the use of intraocular pressure drops. These eye drops can be used short-term, until the pressure is stabilised. Later increases in intraocular pressure can occur as a result of the use of steroid eye drops, which are prescribed routinely after surgery and would usually settle once the steroid drops are stopped.
It is rare for pressure in the eye to remain elevated after a vitrectomy. Only in rare instances will long-term eye drops or surgery be required to alleviate the elevated eye pressure.
Retinal detachment:
There is a 2-3% risk of a retinal detachment occurring after macular hole surgery. If this occurs, in order to preserve vision and limit the extent of loss of vision, you would require retinal reattachment surgery, usually a vitrectomy.
Infection:
As with all surgeries involving the eye, there is an inherent risk of an infection (i.e. endophthalmitis). The risk of endophthalmitis after vitrectomy surgery is lower than that after cataract surgery.
In the first 2 weeks after surgery, eye pain, discomfort, floaters, and eye redness, especially if not settling and increasing, should prompt an immediate visit to your eye doctor to check on your eye, so that early injection of antibiotic treatment into the eye can be administered. If the infection is severe, then vitrectomy surgery to remove infective material from the eye may be required to treat the infection.
There are other intraoperative and post-operative risks aside from the above. Your retinal surgeon will be able to share more details on the potential benefits of vitrectomy surgery with regards to the likelihood of visual improvement. In addition, your retinal surgeon will also be able to provide more information on the risks involved in surgery.



