Diabetic Retinopathy
Singapore has one of the highest rates of diabetes among developed nations globally, with 13% of Singaporeans1 being affected with diabetes! Diabetic retinopathy is one of the major complications of diabetes, and the prime reason why individuals with diabetes suffer from poor vision.
How does diabetes damage the retina?
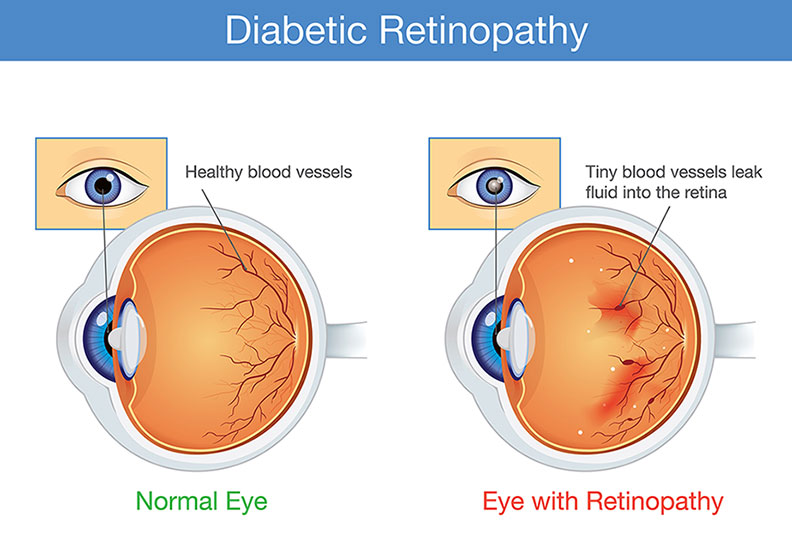
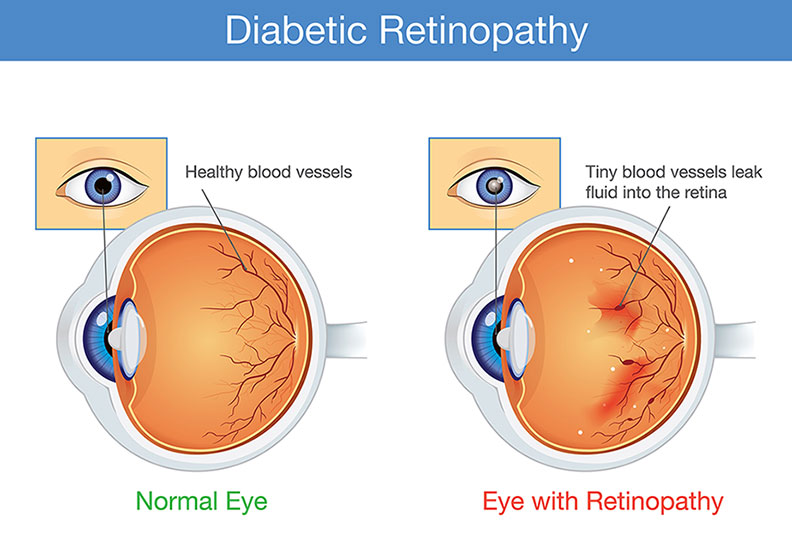
The retina is the important light-sensing structure lining the back of the eye, much like the film in a camera. In order to function well, the retina depends on oxygen supplied by blood circulating through blood vessels.
In diabetes, high blood sugar levels damage the blood vessels of the retina. The damaged blood vessels leak fluid and blood, and as a result, do not provide adequate oxygen and nutrients to the retinal photoreceptor and nerve cells. These cells malfunction and then begin to die. More recent research has shown that diabetes also directly damages the nerves of the retina.
Who is at risk for diabetic retinopathy?
Anyone who has diabetes is at risk of developing diabetic retinopathy. The following factors can increase the risk:
- Duration of diabetes: the longer someone has diabetes, the higher the risk of developing diabetic retinopathy
- Poor control of blood sugar levels
- High blood pressure
- High cholesterol levels
- Pregnancy
How does diabetic retinopathy affect your vision?
The impact on vision due to diabetic retinopathy depends on the stage of the disease.
- Early stage (i.e. non-proliferative) disease
At this stage, diabetic retinopathy has no symptoms. There are micro leaks and bleeding spots in the retina, clinically observable changes in the size and course of blood vessels, however these on their own do not impact vision. - Late-stage (i.e. proliferative) diabetic retinopathy
At this stage, abnormal proliferations of blood vessels form in response to the overall lack of blood and nutrients to retinal tissue. Damage to the blood vessels deprives the retina of oxygen, leading to the production of a signal protein called vascular endothelial growth factor (VEGF).
VEGF promotes the growth of blood vessels from the retina into the vitreous gel cavity. When they bleed, they cause rapid dispersion of blood into the vitreous (i.e. a vitreous hemorrhage), leading to a development of floaters, misty vision, or a partial cloud in the visual field.
Another common complaint of patients with late-stage disease is the reduction of night vision abilities. This is largely because when the retina is starved of nutrients and blood, the photoreceptor cells responsible for night vision don’t function well and die. This gives rise to significant difficulty with driving or functioning at night.
- Advanced proliferative diabetic retinopathy
At this stage, the abnormal blood vessel proliferations form scar tissue that tug on the retina, causing localized areas of retinal detachment. Repeated episodes of bleeding continue and create a vicious cycle of more scarring. Retinal detachments which progress to the macula are vision-threatening and signify a very advanced stage of the disease. Such cases often require surgery in order to preserve vision. A discussion with a retinal specialist is absolutely important to understand the potential risks of surgery undertaken in this scenario, and how soon surgery should be considered.
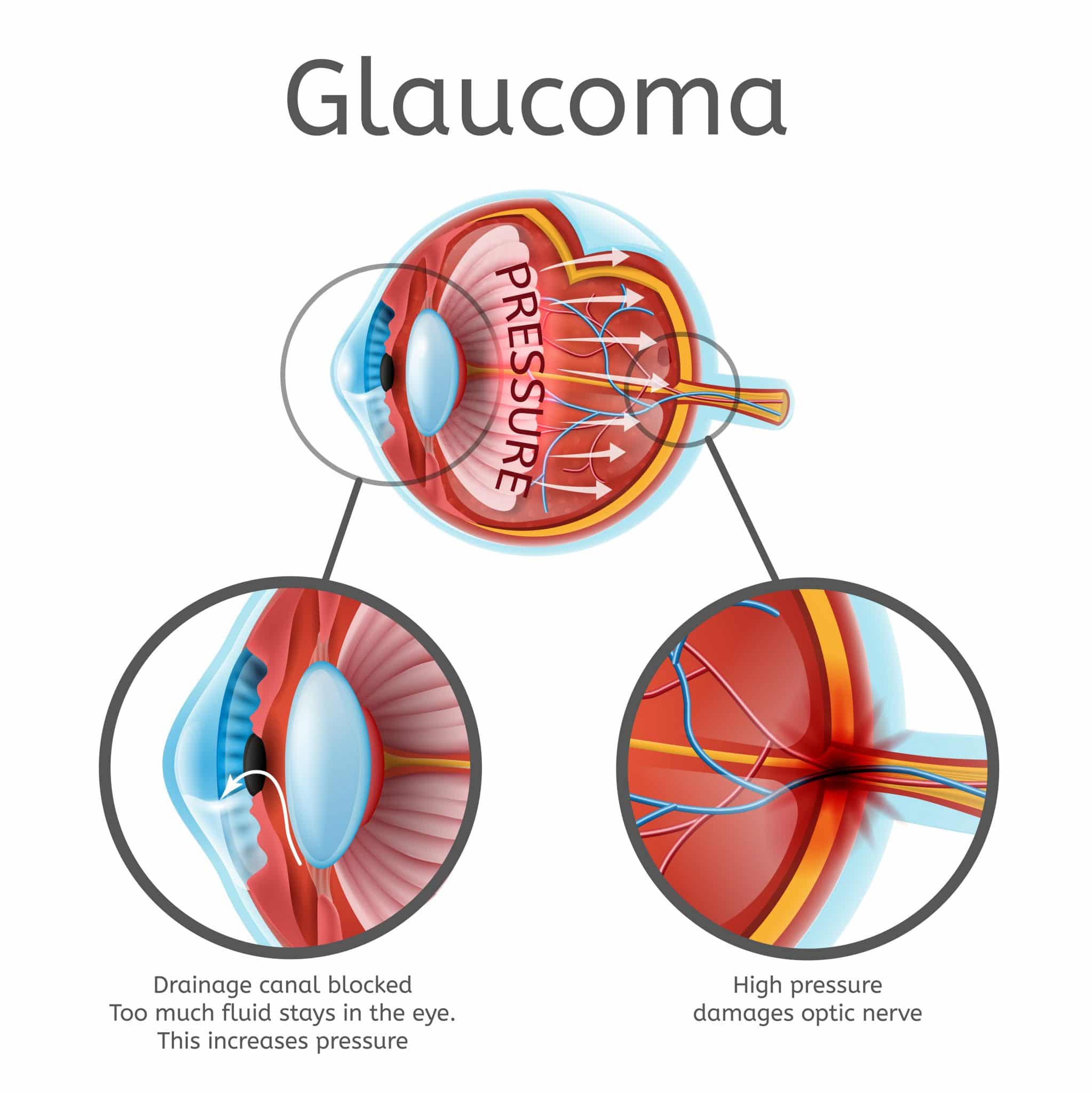
Some advanced cases may also develop proliferation of blood vessels on the iris tissue in the front of the eye as well, causing a specific type of glaucoma, i.e. neovascular glaucoma. The pressures in these eyes are high and vision often poor. Neovascular glaucoma represents a severe end-point of the disease, often requiring both glaucoma and retinal surgery in order to stabilize the eye pressure and prevent further vision loss.
- Diabetic macular edema
Diabetic macular edema can occur alongside non-proliferative or proliferative diabetic retinopathy, and occurs when blood vessels in the macula leak. The macula is the central-most part of the retina, responsible for high-definition and crisp visual quality. Thus, this condition affects central vision, giving rise to a central blur and distorted images.
How do I know if I have diabetic retinopathy?
A comprehensive eye examination by an ophthalmologist is important to make a diagnosis, and consequently treatment, before sight is affected.
Those with type 1 diabetes should see an ophthalmologist once a year, starting five years after the onset of their disease, while those with type 2 diabetes should see an ophthalmologist for a retinal examination soon after their diagnosis, and then schedule annual exams after that.
You may need to see an ophthalmologist more frequently if you are pregnant, or have more advanced diabetic retinopathy.
What happens during an eye examination for diabetic retinopathy?
A dilated fundus examination is essential for your doctor to examine your retina in detail for changes of diabetic retinopathy. This would require the use of dilating eye drops to dilate your pupil.
Further imaging tests are usually conducted as well. The main ones are:
This test sensitively assesses for macular edema. It also gives information about the status of the various nerve cell layers in the retina, and the location of areas in the macula which could be treated before fluid leakage or bleeding.
Additionally, OCT is useful in identifying membranes and scar tissue which often develop in the retina in diabetic retinopathy, and is thus helpful in planning for surgery for these conditions.
A record of your retina is made at each check, which can be helpful in making comparisons at the following visit, especially when there are specific retinopathy changes that need to be closely monitored. With ultra-wide field imaging, a panoramic view of the retina can be captured in a single image.
This is useful to determine if the disease is in the non-proliferative or proliferative phase, and can map out areas of unhealthy retina which should be especially targeted in pan-retinal photocoagulation laser treatment.
Where a good view of your retina is challenging because of significant blood dispersion in the vitreous gel, an ultrasound scan is required to make an assessment of your retinal structural status, and is helpful in planning surgery.
OCT-A is potentially useful in defining the macular blood vessel status, providing information on visual prognosis before commencing any injection or laser treatment.
Can diabetic retinopathy be prevented?
- Good diabetic control (most important factor)
The American Diabetes Association recommends that most people with diabetes keep their A1c level (a measure of average blood sugar levels over the previous two to three months) below 7% to prevent the risk of complications. Better blood glucose control reduces the likelihood of developing diabetic retinopathy, and in patients who have diabetic retinopathy, the severity is lower if the A1c level is better. - Good blood pressure control
Maintaining optimal blood pressure levels are also important in preventing developing diabetic retinopathy. However, once an individual has diabetic retinopathy, it is unclear if controlling blood pressure alters the course of established diabetic retinopathy. - Maintain a good cholesterol level
Managing cholesterol is recommended for overall diabetes management. Although the medical evidence is less clear whether strict cholesterol control also reduces the risk for developing diabetic retinopathy, it makes good sense to also maintain a healthy blood cholesterol level.
How is diabetic retinopathy treated?
The treatment for diabetic retinopathy is highly personalized depending on the severity of disease.
For non-proliferative disease, the mainstay of treatment is close monitoring in the clinic, and improving your overall diabetic control. This alone can be successful in reversing many of the non-proliferative changes, such that you do not reach the point of requiring treatment.
However, significant macular edema and proliferative diabetic retinopathy need treatment. There are multiple other factors which your eye doctor may take into consideration in planning your treatment:
- Overall activity or stability of diabetic retinopathy (i.e. how likely and how soon it is that the retinopathy will worsen)
- Severity of vision loss
- Presence, severity, and configuration of macular edema
- Visual prognosis with and without treatment
- Presence of a cataract
- Other eye conditions which may affect the outcome of treatment or contraindicate some treatments
- Whether you are pregnant
- Your preferences regarding treatment type
- Your ability to maintain regular follow-up treatment
- Your overall diabetic control
In general, the following are several treatment modalities:
For macular edema:
- Anti-VEGF medications: These are medications that can bind VEGF molecules and prevent its negative impact on blood vessel leak and growth. These “anti-VEGF” agents are injected directly into the eye in an “intravitreal injection”. It improves diabetic macular edema, as well as the severity of diabetic retinopathy.
- Intravitreal steroid injections: In some patients whose macular edema is resistant to anti-VEGF injections, steroids injected directly into the eye may allow better control of fluid leakage and improve vision. The downside of steroid injections is the risk of a pressure rise, and thus need for monitoring and treatment if this develops.
- Macular laser treatment: the laser beam targets leaking and bleeding spots, as well as encourages the natural removal of macular edema fluid by the eye. Treatment effects usually take longer than that of intravitreal anti-VEGF agents.
- Vitrectomy surgery with membrane peeling: in cases where there are membranes on the retina causing the edema, vitrectomy surgery may be an option in improving the macular profile and vision.
For proliferative diabetic retinopathy:
- Laser panretinal photocoagulation treatment: Multiple spots of laser are applied to unhealthy retina. This has been the mainstay of treatment for many years, and up to this day is still effective and a relevant form of treatment. As strange as it may sound, laser reduces the amount of unhealthy retina actually reduces the abnormal drive to VEGF production, reducing the risk for abnormal blood vessel growth.
- Anti-VEGF injections: Regular injections of anti-VEGF agents to the eye are an alternative to panretinal laser treatment, or as a temporizing measure to reduce blood vessel proliferation. The downside is the need for regular treatment.
- Vitrectomy surgery: Vitrectomy surgery can be employed in several situations in proliferative disease. It is often performed to clear our dense vitreous hemorrhages that do not resolve after a period of observation, especially if there is some urgency to remove the blood in order to perform laser photocoagulation. Vitrectomy surgery with scar tissue removal is also the only means of treating retinal detachments progressing towards the macula.
With several different treatment modalities available, it is important that you obtain a discussion with your eye doctor specific to your situation, in order to make an informed decision. Each treatment has its pros and cons, and the specific treatment recommended in your case will need to carefully balance all these considerations.
The silver lining in the treatment of diabetic eye disease in the modern era is that with a vast armamentarium of treatment options, diabetic patients are detected earlier and have much better outcomes with treatment, compared to patients just 10 or 20 years ago. Thus, instead of preventing loss of vision, we are now moving towards improving vision.