The Shadow in My Eye: Could It be a Retinal Detachment?
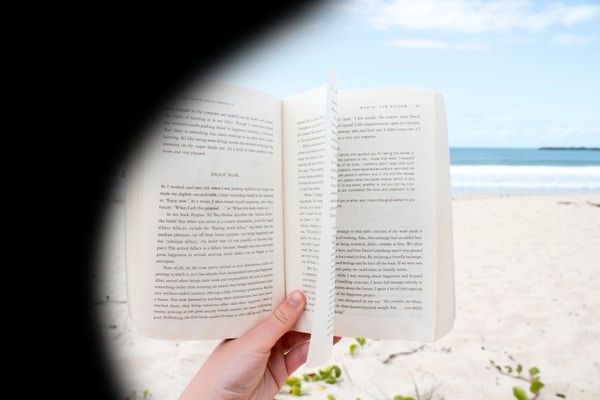
Most of us would have some vague idea that a retinal detachment is a very severe eye condition, with the possibility of significant and permanent loss of vision. The symptoms one hears about are undoubtedly terrifying, with often-mention of sudden and countless floaters, persisting flashing lights, and an abrupt curtain-like darkening of vision coming in from the side.
With current treatment methods for retinal detachments, many retinal detachments can be successfully treated to achieve the best possible outcomes.
What is a Retinal Detachment?
The retina is the all-important light-sensing structure in the eye that lines the back wall of the eye. It is much like the old-school film in a conventional camera, absorbing and transmitting light to the brain via the optic nerve. This transmission gives rise to the visual images that we see.
Simply put, a retinal detachment occurs when the retina peels away from the wall of the eye.
Why does a Retinal Detachment Happen?
To answer this question, we need to consider the 3 main forms of retinal detachments.
1. Rhegmatogenous detachments, which develop from retinal tears
The vitreous gel in our eyes softens and becomes more liquefied as we age. As the vitreous gel is quite firmly attached to the retina, it tugs on the retina and generates the visual sensation of flashing lights. Now, if the vitreous gel body separates from the retina with sufficient force, a retinal tear results. The development of a new retinal tear then heralds symptoms such as a sudden onset of numerous floaters. If the retinal tear is detected at this stage, treatment in the form of laser retinopexy or cryotherapy freezing treatment can be applied to seal the tear, significantly reducing the risk of progression of the retinal tear.
However, if the retinal tear is left untreated, vitreous fluid will eventually find its way through the tear, ultimately lifting the retina off the wall of the eye, and leading to a retinal detachment. The majority of retinal detachments require surgical treatment. Early detection and preventive treatment of retinal tears is therefore highly important.
2. Tractional retinal detachments, which develop from scarring on the retinal surface
Scarring on the retinal surface slowly and progressively tug on the retina and lift it off the wall of the eye. The common causes of such scarring include advanced diabetic retinal disease, prior retinal vein occlusions, and inflammatory eye disease affecting the retina and vitreous. In all these diseases, scarring develops as a late complication, and so it is usually after many years of having had the disease that patients develop tractional detachments.
3. Exudative detachments, which occur when fluid leaks under the retina
Exudative retinal detachments are caused by fluid leakage beneath the retina, which may arise from abnormal retinal blood vessel networks, choroidal or inflammatory eye disorders, or tumors in the eye.
How would I Know if I Have a Retinal Detachment?

Rhegmatogenous retinal detachments are the most common, and often present with a distinct set of symptoms that all individuals should be aware of.
If you experience the following warning signs of retinal detachment, it is important that you seek medical evaluation on an urgent basis:
- Seeing numerous floaters (seen as spots or flecks or a haze)
- Seeing flashing lights
- Experiencing a shadow or curtain from the side of your vision,
slowly extending to the centre, ending with blurred central vision
In a minority of cases of rhegmatogenous retinal detachments, the individual might actually be unaware of the disease, as there are no symptoms unless the detachment progresses. This is because the earlier stage of these retinal detachments affects the corners and not the central part of the retina (i.e. the macula).
It is only when the retinal detachment worsens and progresses to involving the macula, that the impact to the vision is felt.
Am I at Risk for a Retinal Detachment?
While older age is a risk factor, there are other factors that could put you at risk for a retinal detachment, including:
- Short-sightedness (myopia)
- Known retinal degenerative changes, e.g. lattice degeneration
- Prior eye surgery such as cataract surgery
- Prior eye trauma
- Family history of retinal tears or detachment
Can Retinal Detachments be Treated?
For all cases of retinal detachments, the objective is to reattach the retina and to achieve the best possible vision. Unlike a retinal tear, which can be treated with laser retinopexy or freezing cryotherapy, most retinal detachments require surgery.
There are 4 key approaches to reattaching the retina. These methods are: vitrectomy, scleral buckle, pneumatic retinopexy, which are surgical methods, and laser retinopexy, which is solely a laser procedure.
These procedures are usually performed in the operating theatre. Your surgeon will advise if local or general anesthesia is required. Learn more about what each treatment involves here.
There will be certain cases where a combination of procedures is used (e.g. a vitrectomy combined with a scleral buckle, or a scleral buckle and pneumatic retinopexy). Your retinal specialist will recommend the treatment option that is most tailored to your condition.
Can a Retinal Detachment affect my Vision even after Treatment?
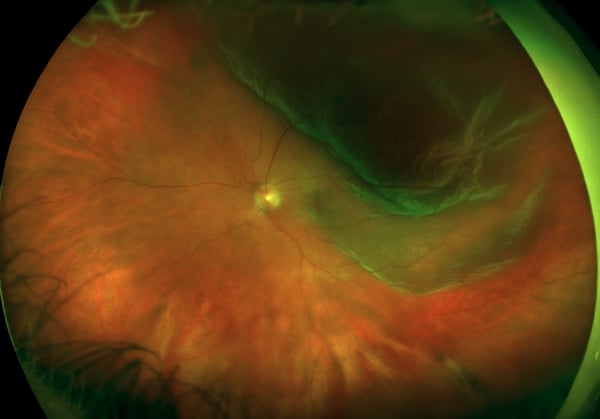
A retinal detachment demonstrating involvement of the macula by the retinal detachment.
The extent to which suffering from a retinal detachment impacts your vision in the longer-term, even after the retina is successfully reattached with surgery, would depend on how much of the macula is affected by the detachment in the first place, and for how long the macula has been detached.
The macula is important because it is responsible for high-definition vision that allows one to appreciate fine contrast, color, recognize faces, and precise detail.
So in eyes in which the macula is involved in the detachment, restoration of these visual abilities will not be complete, even after the retina is reattached back into position.
Scenario 1: Your macula is intact
In the majority of cases, you will likely restore all of your prior vision and visual quality after treatment in the longer-term.
Scenario 2: Your macula was detached, but only for a short time
Your longer-term vision may be affected slightly, in terms of color, size, contrast, and distortion of objects, but overall level of vision and visual quality does somewhat approximate pre-detachment levels.
Scenario 3: Your macula has been detached for a significant time period
The recovery of vision will likely not be as favorable, compared to the above two scenarios, but it is certainly possible that you will still benefit from an improvement in vision.
Regardless of the visual or structural prognosis of your retinal detachment, it is still important to seek an ophthalmologist for assessment and treatment of your condition, because progression to total loss of vision in the longer-term is an absolute certainty if left untreated.
Conclusion

A retinal detachment is a potentially sight-threatening condition, however current medical technology and surgical techniques offer patients the best chances of preserving their vision.
The development of a retinal tear or detachment heralds several key symptoms that all individuals should be aware of. It is important to know that early assessment by an ophthalmologist, and expedient treatment can save your vision. If you have any of the above mentioned symptoms, do not wait for a later appointment to see an eye specialist as a delay in treatment, even if for just a few hours, can make all the difference between preserving or losing your pre-detachment level of vision.
Request for an eye examination today.

Tel: +65 6836 1000
Whatsapp: +65 9843 1000
For general enquiries and appointment only
Email: [email protected]
Monday to Friday: 9am to 6pm
Saturday: 9am to 4pm
*Last Registration Time 2pm
Sunday & PH: Closed












